CRYOLIPOLYSIS WITH A DOUBLE-APPLICATOR 3-DIMENSIONAL COOLING CUP DEVICE
Dr Adrian Lim MBBS FACD FACP
Royal North Shore Hospital, uRepublic Cosmetic Dermatology and Veins NSW Australia
Contents
INTRODUCTION
There is a strong consumer demand for non-invasive body contouring through localised fat reduction. Lasers, radiofrequency, acoustic wave and focused ultrasonic cavitation are currently available options for this purpose. Since 2005, suction-assisted cryolipolysis (fat freezing) has become one of the most popular techniques for body contouring with many studies supporting its safety, efficacy and reliability. As a result, consumers and practitioners globally have embraced this method of focal body contouring. In late 2015, the Australian Therapeutic Goods Administration (TGA) approved a new cryolipolysis device with two applicators with 3-dimensional surround cooling cup (CLATUU) for body contouring. The primary objective of this study is to assess efficacy and safety of localised fat reduction with CLATUU. The secondary objective is to compare and evaluate the different body contour measuring techniques – standardised photography, calliper measurement, circumference tape measurement, ultrasound measurement and patient self-assessment – in their validity and reliability in monitoring patient progress following cryolipolysis.
The primary objective of this study is to assess efficacy and safety of localised fat reduction with CLATUU. The secondary objective is to compare and evaluate the different body contour measuring techniques – standardised photography, calliper measurement, circumference tape measurement, ultrasound measurement and patient self-assessment – in their validity and reliability in monitoring patient progress following cryolipolysis.
METHODS
8 consecutive treatment-eligible patients were enrolled into the cryolipolysis study for prospective evaluation over a 4-month follow-up period. Patients with localised fat accumulation on the trunk and proximal limbs were included in the study. Patients with global obesity, cold intolerance such as Raynaud’s, and connective tissue diseases such as morphea or lupus panniculitis, and patients with previous previous invasive (liposuction) or non-invasive methods of localised fat reduction procedures were excluded from the study. Patients were requested to maintain a constant weight over the study period (keeping within 3kg of baseline weight) and to maintain their current level of physical activity.
The target sites were patient initiated to reflect real-life clinical setting and the location recorded with X and Y axis using the umbilicus as the fixed reference point. All trial patients had the option of treating either single-site or 2-sites simultaneously (e.g. lateral abdomen and one inner thigh). Baseline assessment involved 6-view body photography (anterior, posterior, right anterolateral, left posterolateral, right lateral, left lateral), weight, circumference tape measurements, calliper measurements and M-mode ultrasound measure of adipose tissue thickness (mean of 12 different measurements points taken within the treatment area). All trial patients were followed-up at 2 months and 4 months for similar measurements. In 2 patients with symmetrical bilateral fat accumulation, the contralateral site served as internal control. The trial patients had the option of treating 2– sites at the one time e.g. lateral abdomen and inner thigh. Trial patients were also offered the option of a repeat treatment to the same area with a minimum interval of 2 months between treatments. The clinical measurements were undertaken by the same nurse practitioner and the ultrasound measurements were performed by the same sonographer (Toshiba).
All trial patients were treated with a standard protocol at the nominated ‘problem’ site(s). The treatment protocol involved initial prior application of a matrix gel pad followed by application of either a flat or wing (curved) suction cup depending on the body location and contour. The parameters were suction (step 4), cooling (step 4) and duration of one hour. Two months after the final treatment, patients were surveyed about their experience and satisfaction of the procedure, including self-rating of perceived degree of fat reduction post-treatment. At the end of the study, two blinded dermatologists rated the baseline, 2-months and 4- months photographs for all the trial patients according to a 4-point scale: no change (0%), mild reduction (< 25%), moderate reduction (25-50%) and marked reduction (>50%).
RESULTS
The subject demographics were: 6 females and 2 males, age range: 36 – 60 years old (mean: 46.8 years old). One subject was excluded from the study because of an unrelated traumatic injury to the shoulder requiring surgery. Of the 7 subjects, a total of 13 sites were treated: 3 subjects requested treatment at 2 body sites, 2 subjects had 1 site treated, and 1 subject had 4 sites treated. The lateral abdomen was the most commonly nominated site (figure 1). The specified measurements were done at baseline, 2-months and 4-months post-treatment (table 1). The most consistent record of body contouring change was photographic assessment and ultrasonic fat measurements, where the mean global ultrasonic fat reduction across all subjects was -19.44% (control: +0.62%) (table 1). Fat reduction across the 3 treatment groups (control, single treatment, double treatment) appear to correlate with the ultrasound measurements of +0.62%, -16.43% and -19.44% respectively. The calliper and circumference measurements correlated poorly with the clinical changes, with mean global reduction of -5.54% and -0.31% respectively for the enrolled subjects. Independent blinded physician (dermatologists) assessment of localised fat reduction was -30.0% after 1 treatment and -39.5% after 2 treatments, based on a mean 4-point rating scale (table 1). There was close concordance between the blinded dermatologists global score: 1.45 and 1.36 (mean 1.41), representing a mean global reduction of -35.2% on the 4-point rating scale (control: -12.5%).
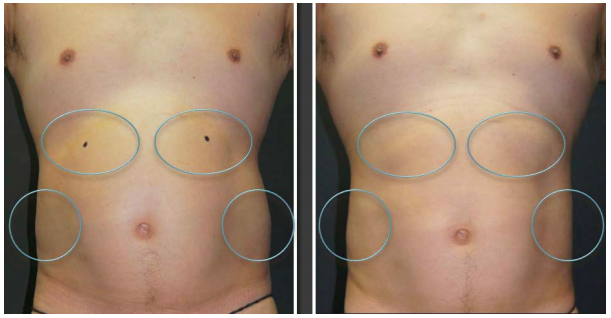
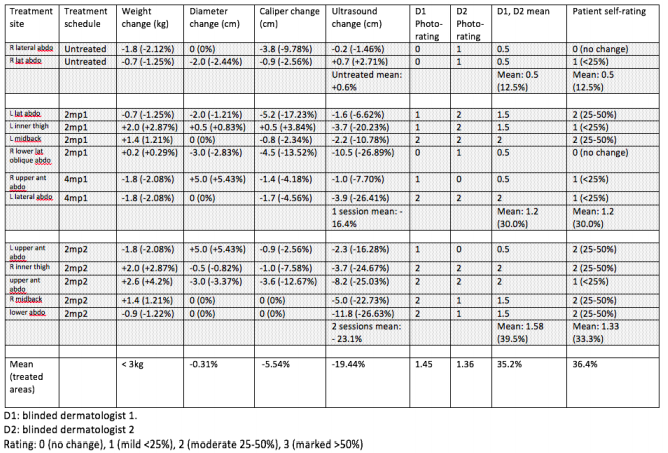
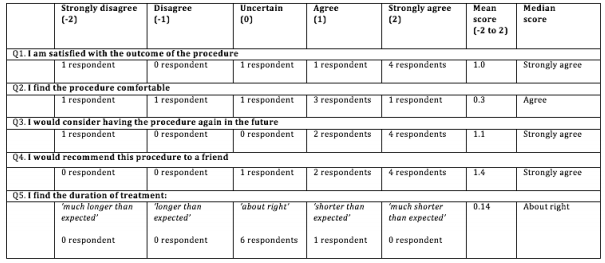
The patient satisfaction survey at 2-months post-treatment revealed 71.4% (5 out of 7 patients) either ‘agreed’ or ‘strongly agreed’ that the outcome was satisfactory (table 2). Five patients elected to have a repeat treatment on the same area 2 months after the initial treatment. Of the 2 dissatisfied patents, one felt that there was ‘no change’ post-procedure but revised her self-assessment to ‘marked reduction’ upon reviewing the before-after photos (figure 2). The overall patient self-assessment showed concordance with blinded physician assessment: -36.4% and -35.2% respectively on the 4-point rating scale (Rating: 0 [no change], 1 [mild <25%], 2 [moderate 25-50%], 3 [marked >50%]).
DISCUSSION
In the last few years there has been a marked increase in interest and uptake of cryolipolysis for localised fat reduction. One study showed an 823% increase in cryolipolysis procedures over a 3-year period: 201 patients treated in the first year, 671 patients in the second year and 1857 patients in the third year, highlighting the business case for offering the service.1 Other non-surgical options for localised fat reduction include high intensity focused ultrasound, unipolar radiofrequency, acoustic wave therapy and and laser therapy, but these do not compare as favourably as cryolipolysis in terms of efficacy, safety and tolerability.2
In one study with 42 patients, 79% noticed fat reduction on themselves at 2-4 months.3 Another study with 50 patients, 89% showed a noticeable improvement on photography with a similar proportion (80%) being happy with the results at 6 months.4.5 Most studies indicate a fat reduction of approximately 20 – 25% – either on calliper or ultrasonic measurements – 3 to 6 months after a single treatment session. 6.7 Two treatments appear to result in greater fat reduction than a single treatment session: 28.5% versus 19.7%.8 Boey et al demonstrated a 44% increase in fat loss with 2 minutes of massaging immediately post cryolipolysis, and this manoeuvre has become standard practice in most centres.9 Carruthers et al speculated on possible skin tightening effects post cryolipolysis based on a series of 14 patients.10
The safety of cryolipolysis has been well established. Cryolipolysis is not associated with any alterations in serum lipids and liver function. 11 Dysaesthesia (numbness) has been reported to occur in up to 73% of patients lasting 3 weeks although 18% of cases may persist up to 3 months. 12 The dysaesthesia is self-limiting and peripheral nerve biopsy and confocal microscopy did not show any alteration in the neural network.13 There was a single reported case of paradoxical fat hypertrophy that started at 3 months and stabilised at 5 months and the incidence of this event has been estimated to be 1: 20,000.14
Our study showed no adverse effects associated with CLATUU cryolipolysis. Our subjects experienced an initial ‘suction’ discomfort lasting 5-10 minutes followed by cold-induced numbness for the rest of the procedure. The most common post-treatment effect was numbness lasting from 1 to 3 weeks. One patient with atopic dermatitis experienced mild itching over the treated site for a few days post-cryolipolysis.
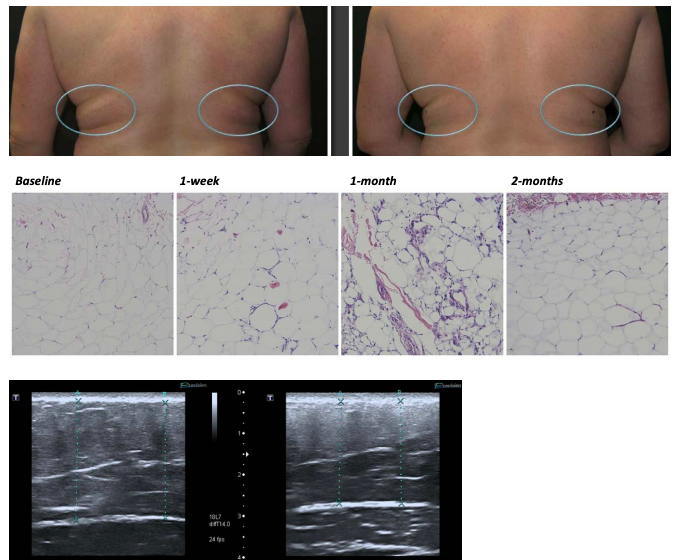
One patient had serial skin biopsies at baseline, 1-week, 1-month and 2-months post cryolipolysis revealing an inflammatory response that was mild at 1 week, marked at 1 month and fully resolved at 2 months (figure 3a, b) with corresponding ultrasound measurement images of the left upper postero-lateral flank (figure 3c). Patients will typically notice localised fat loss over the treated area at 2 months, but as early as 1-month postprocedure.
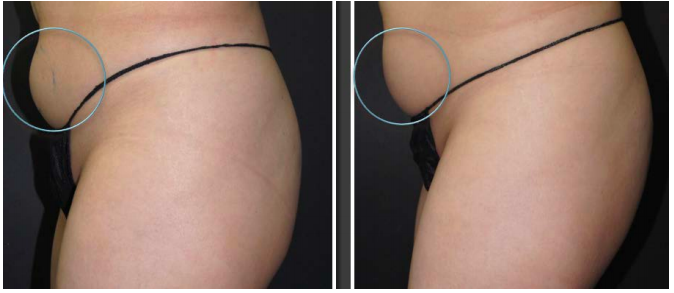
Our pilot study on various methods of tracking fat reduction favour standardised photography and ultrasound over callipers and circumferential tape measure. Circumferential tape measurement of abdominal girth is unlikely to be reliable given the limited target area in the context of the much larger truncal girth, which expands and contracts with the breathing cycle. We were unable to demonstrate consistency with calliper measurements of skin fold thickness, which can be pinch- and pressure- sensitive and prone to early user-error. Photography performs well on reliability, familiarity and accessibility, and furthermore, allows meaningful before-after comparison for patients. The anterior (front-on) and side (lateral) profile views are particularly useful to demonstrate contour changes. Oblique views may not highlight contour changes adequately and this was highlighted by one patient who was uncertain about the outcome and remained unconvinced on review of post-treatment oblique photos despite a 26.9% fat thickness reduction on ultrasound (figure 4). This case illustrates how improper patient selection (high body mass index) and site selection (non-obvious fat bulge) can lead to patient dissatisfaction.
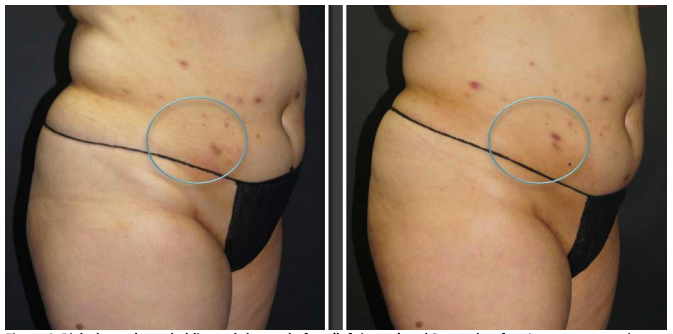
Ultrasonic measurement of fat loss is essentially a research tool with significant accessibility and technical issues for most clinicians. Fat thickness measurement with the ultrasound probe is susceptible to probe-pressure and patient-posture variations (lying/ sitting/ standing) and these are likely explanations for the apparent underestimate of the global fat reduction (19.44%) relative to photographic assessment. Photographic representation of body contour can also be influenced by several factors including camera angle, lighting, patient stance, posture and breathing cycle. Nevertheless, standardised photography remains a valuable tool for monitoring post-cryolipolysis progress and provided one subject with valuable photo-documentation of visible fat reduction (figure 2).
The limitations of this study are a relatively small sample size, a predominance of torso (abdominal) treatment sites and potential investigator bias from using an industry sponsored device (Cryomed Australia).
CONCLUSION
Cryolipolysis with CLATUU is a safe effective procedure for localised fat reduction with a high patient satisfaction rate. Standardised photography is recommended as an effective monitoring tool and documentation of post-cryolipolysis progress.
REFERENCES
- Stevens WG, Pietrzak LK, Spring MA. Broad overview of a clinical and commercial experience with CoolSculpting. Aesthet Surg J. 2013 Aug 1;33(6):835-46
- Krueger N, Mai SV, Luebberding S, Sadick NS. Cryolipolysis for noninvasive body contouring: clinical efficacy and patient satisfaction. Clin Cosmet Investig Dermatol. 2014 Jun 26;7:201-5.
- Rosales-Berber IA, Diliz-Perez E. Controlled cooling of subcutaneous fat for body reshaping. Presented at the 15th World Congress of the International Confederation for Plastic, Reconstructive and Aesthetic Surgery, 2009, New Delhi, India.
- Kaminer MW, Newman J, Allison J. Visible cosmetic improvement with cryolipolysis: Photographic evidence. Paper presented at: 2009 Annual Meeting of the American Society for Dermatologic Surgery: October 1-4, 2009; Phoenix, Ariz.
- Dover J, Kaminer M, Teahan M, Barrett L. Patient satisfaction at 2 and 6 months after a single non-invasive cryolipolysis treatment for subcutaneous fat layer reduction. Lasers Surg Med. 2011;43:968.
- Sasaki GH, Abelev N, Tevez-Ortiz A. Noninvasive selective cryolipolysis and reperfusion recovery for localized natural fat reduction and contouring. Aesthet Surg J. 2014;34:420– 431.
- Dierickx CC, Mazer JM, Sand M, Koenig S, Arigon V. Safety, tolerance, and patient satisfaction with noninvasive cryolipolysis. Dermatol Surg. 2013 Aug;39(8):1209-16.
- Pinto HR, Garcia-Cruz E, Melamed GE. A study to evaluate the action of lipocryolysis. Cryo Letters 2012;33:177–181.
- Boey GE, Wasilenchuk JL. Enhanced clinical outcome with manual massage following cryolipolysis treatment: a 4-month study of safety and efficacy. Lasers Surg Med. 2014 Jan;46(1):20-6. 2013.
- Carruthers J, Stevens WG, Carruthers A, Humphrey S. Cryolipolysis and skin tightening. Dermatol Surg. 2014 Dec;40 Suppl 12:S184-9.
- Riopelle JT, Kovach B. Lipid and liver function effects of the cryolipolysis procedure in a study of male love handle reduction. Lasers Surg Med. 2009:82.
- Garibyan L, Sipprell WH III, Jalian HR, Sakamoto FH, Avram M, Anderson RR. Three dimensional volumetric quantification of fat loss following cryolipolysis. Lasers Surg Med. 2014;46:75–80.
- Coleman SR, Sachdeva K, Egbert BM, Preciado J, Allison J. Clinical efficacy of noninvasive cryolipolysis and its effects on peripheral nerves. Aesthetic Plast Surg. 2009 Jul;33(4):482-8.
- Jalian HR, Avram MM, Garibyan L, Mihm MC, Anderson RR. Paradoxical adipose hyperplasia after cryolipolysis. JAMA Dermatol. 2014 Mar;150(3):317-9.



